Vasectomy has long been recognized as one of the most reliable and permanent methods of male contraception. Over the past several decades, the introduction of the no scalpel vasectomy (NSV) technique has revolutionized male sterilization by making the procedure less invasive, safer, and more widely acceptable. Developed in China in the mid-1970s and introduced to the United States in the 1980s, this approach avoids large incisions, instead using a small puncture to access and occlude the vas deferens.
The simplicity, effectiveness, and reduced recovery time of no scalpel vasectomy have made it an increasingly attractive option worldwide. However, its global clinical adoption has not been uniform. Cultural, economic, medical, and policy-related factors shape how different regions embrace or resist this minimally invasive technique.
This article explores the journey of no scalpel vasectomy: global clinical adoption, focusing on regional trends, barriers, patient perceptions, and future directions.
The Evolution of No Scalpel Vasectomy
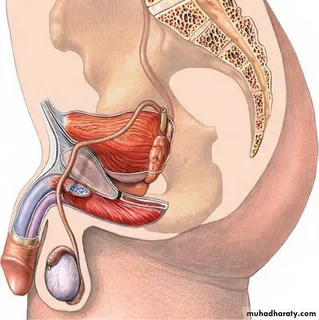
Traditional vasectomy involved a scalpel incision, often requiring sutures, with associated risks of bleeding, infection, and scarring. In contrast, no scalpel vasectomy employs a sharp-tipped instrument to puncture the skin, spread tissue gently, and expose the vas deferens. The vas is then occluded through cauterization, clips, or fascial interposition.
Benefits of NSV include:
- Reduced pain and discomfort
- Lower risk of infection and hematoma
- Minimal scarring
- Faster recovery times
- High patient satisfaction rates
These advantages have driven its expansion beyond China to virtually every continent.
Global Trends in Clinical Adoption
1. Asia
The birthplace of NSV, Asia remains at the forefront of adoption.
- China: The technique was pioneered here as part of national family planning strategies. By the 1990s, millions of procedures were performed annually. However, in recent years, vasectomy rates have declined due to policy changes that relaxed the one-child rule.
- India: India has actively promoted NSV as part of government-sponsored sterilization programs. Training camps and public health campaigns have encouraged men to consider the procedure, although uptake still lags behind female sterilization.
- Southeast Asia: Countries like Thailand and Indonesia have integrated NSV into community-based health initiatives, often supported by NGOs such as Marie Stopes International.
2. North America
- United States: NSV was introduced in the 1980s and has since become the dominant vasectomy technique. Adoption is driven by patient demand for minimally invasive options and physician training programs that emphasize NSV’s advantages. However, overall vasectomy rates remain lower than female sterilization in the U.S.
- Canada: Adoption has been high, with vasectomy being one of the most common contraceptive methods among Canadian men. The majority of vasectomies performed in Canada are no scalpel techniques.
3. Europe
- Western Europe: NSV is widely accepted in countries like the UK, Netherlands, and France, where strong healthcare systems and cultural openness to male contraception support its use.
- Eastern Europe: Adoption is slower, with vasectomy rates generally low due to cultural resistance and limited availability of trained providers.
4. Latin America
- Brazil, Mexico, and Colombia have seen growing adoption of NSV as part of broader reproductive health programs. Cultural attitudes toward male sterilization remain mixed, but urban populations are increasingly embracing the method.
5. Africa
NSV adoption in Africa has been slower due to limited infrastructure, cultural barriers, and prioritization of female sterilization in family planning programs. However, international organizations are working to expand training for African surgeons to introduce NSV as a safer and more acceptable option.
6. Oceania
- Australia and New Zealand have some of the highest vasectomy rates in the world, with NSV being the standard of care. Cultural acceptance and robust healthcare access make these regions leaders in global adoption.
Factors Influencing Global Adoption
1. Cultural Perceptions of Masculinity
In many societies, vasectomy is associated with misconceptions about masculinity, libido, or strength. These cultural beliefs significantly slow down NSV adoption, especially in Latin America, Africa, and South Asia.
2. Government and Policy Support
Countries that integrate vasectomy into national health policies (e.g., India, Canada, UK) see higher adoption rates. Conversely, where vasectomy is not actively promoted, NSV remains underutilized.
3. Access to Training and Skilled Providers
One of the biggest barriers is the lack of trained healthcare providers. NSV requires specialized training in minimally invasive techniques. Regions without sufficient training programs face slower adoption.
4. Public Awareness and Education
Adoption is strongly linked to patient awareness. In areas where public health campaigns emphasize NSV’s safety and benefits, more men are willing to consider it.
5. Healthcare Infrastructure
Countries with strong primary healthcare systems (e.g., Canada, UK, Australia) can deliver NSV more efficiently than those with underfunded systems.
Comparative Success Rates
Across the globe, studies show that no scalpel vasectomy is at least as effective as traditional vasectomy, with fewer complications. Key findings:
- Effectiveness: >99% success in preventing pregnancy.
- Complications: Lower rates of hematoma, infection, and pain compared to traditional vasectomy.
- Patient Satisfaction: High across multiple regions, with reports of quicker recovery and less postoperative discomfort.
Case Studies in Global Adoption
China – A Policy-Driven Beginning
China was the pioneer, using NSV as a cornerstone of its family planning strategy. Tens of millions of procedures were performed, setting the stage for global recognition.
United States – A Patient-Driven Market
In the U.S., clinical adoption was propelled not by government policy but by patient demand for less invasive procedures and the willingness of urologists to embrace innovation.
India – Public Health Promotion
Government programs promoting NSV have increased awareness, but uptake remains lower than female sterilization, indicating persistent gender-based contraceptive expectations.
Africa – Emerging Adoption
Pilot projects in Kenya and South Africa have shown that, with proper education and access, men are receptive to NSV. However, scaling remains a challenge.
Barriers to Wider Global Adoption
- Persistent Myths – Beliefs that vasectomy causes impotence or weakness still deter men.
- Gendered Responsibility – Contraception is still largely viewed as a woman’s responsibility in many cultures.
- Religious Opposition – Certain faith traditions discourage sterilization, limiting uptake in conservative regions.
- Economic Priorities – In low-income countries, resources are often directed toward female sterilization, considered more cost-effective.
The Role of International Organizations
NGOs and international health organizations play a crucial role in global adoption by:
- Providing NSV training workshops.
- Running community awareness campaigns.
- Offering subsidized or free procedures in underserved areas.
- Collaborating with governments to integrate NSV into reproductive health policy.
The Future of No Scalpel Vasectomy in Global Health
- Expansion of Training Programs – Increasing the number of trained providers in Africa, South Asia, and Eastern Europe.
- Integration into Telemedicine – Remote consultation and postoperative follow-up could increase acceptance in rural areas.
- AI and Robotics – Future innovations may make NSV even less invasive and more precise.
- Shifting Gender Norms – As cultural views evolve, more men may share contraceptive responsibility, normalizing vasectomy.
- Policy Support – National governments that actively include NSV in public health initiatives are likely to see the fastest adoption rates.
Conclusion
The story of no scalpel vasectomy: global clinical adoption highlights both progress and persistent challenges. From its origins in China to its widespread acceptance in North America, Europe, and Oceania, NSV has proven itself as a safe, effective, and patient-friendly option. Yet, adoption remains uneven due to cultural, social, and infrastructural barriers.
As awareness grows and training expands, NSV has the potential to play a transformative role in global family planning. Encouraging male participation in contraception not only balances reproductive responsibility but also empowers couples with safer, more equitable options for long-term fertility control.
FAQs
1. Is no scalpel vasectomy available worldwide?
Yes, NSV is available in many countries, but access varies. It is common in North America, Europe, and Oceania, but less accessible in parts of Africa, South Asia, and Latin America due to limited provider training and cultural resistance.
2. Why is no scalpel vasectomy preferred over traditional vasectomy?
NSV is less invasive, causes less pain, has lower complication rates, and offers quicker recovery while maintaining the same high effectiveness in preventing pregnancy.
3. What factors slow down global adoption of no scalpel vasectomy?
Cultural beliefs, gender norms, religious opposition, and lack of trained healthcare providers are the main barriers to widespread adoption.